Many autistic people experience gastrointestinal (GI) issues, such as constipation and abdominal pain. Still unknown, though, was whether GI problems themselves might contribute to the differences in social behaviors that are associated with autism.
Now, research in mice has found that repeated GI irritation can make individuals less socially active, even after GI symptoms have completely subsided. What’s more, specific species of bacteria found in the human gut can help prevent GI irritation and the related changes in social behavior.
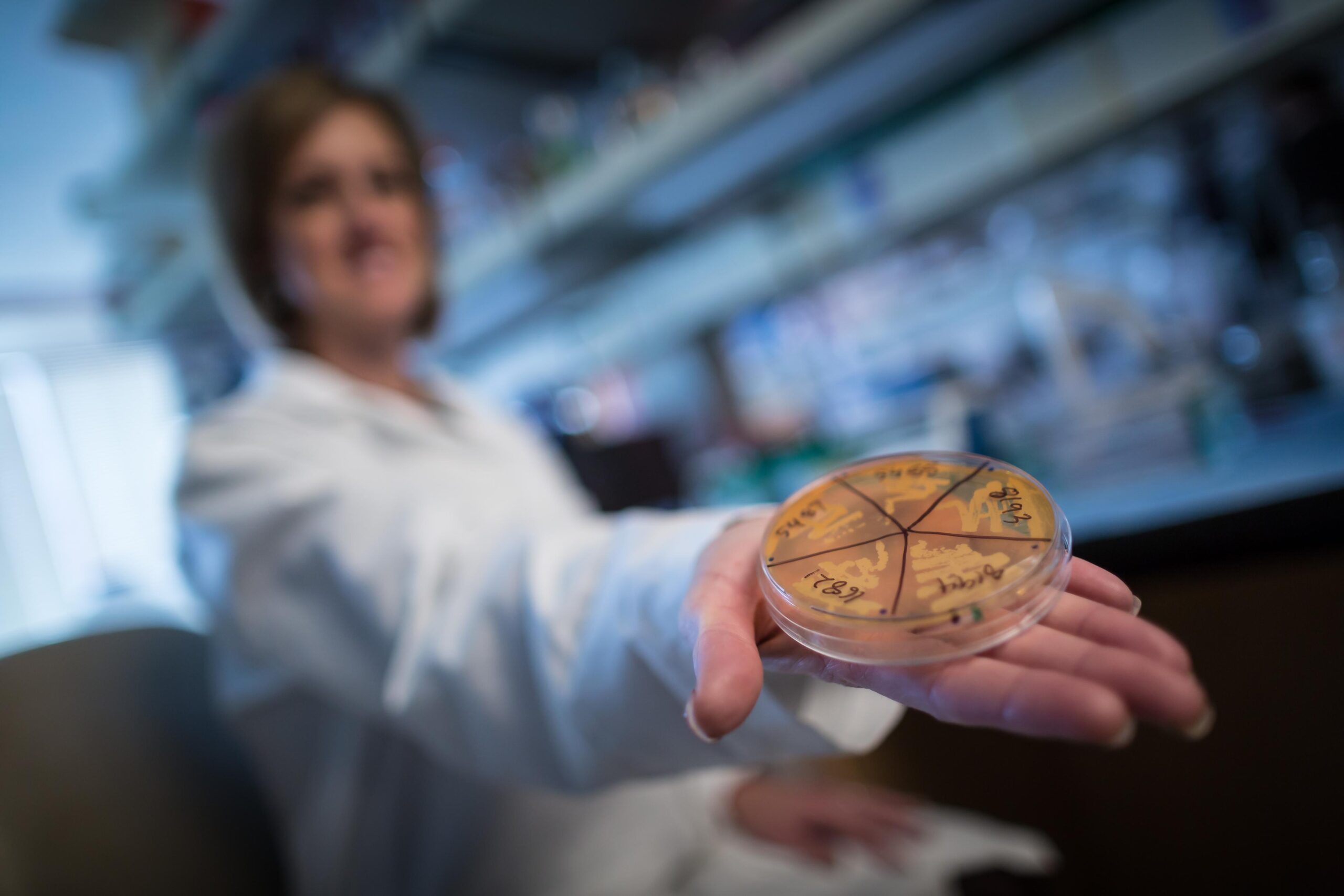
To figure out how GI problems influence social behavior, the researchers looked at mice that had colitis, a condition in which the gut is inflamed and damaged. Mice are social animals, which makes them indispensable for studying simple social behaviors.
Unsurprisingly, mice that were actively experiencing colitis symptoms had altered behavior. But even after the colitis had resolved and the animals returned back to health, mice that had experienced past bouts of colitis were less likely to spend time interacting with a new mouse.
Gut health and behavior can be profoundly influenced by the bacteria that live in the gut, which prompted the researchers to ask whether differences in gut bacteria might affect the GI symptoms and behavioral differences associated with autism. The researchers transplanted gut bacteria from autistic people or their neurotypical (not autistic) relatives into mice. They found that when mice carried gut bacteria from autistic people, the mice often had more severe GI symptoms in response to gut irritation.
Next, the scientists took a closer look at individual species of gut bacteria to see which might be responsible for the changes in gut health. They noticed that neurotypical people tended to have more of a specific type of bacteria called Blautia. When the researchers inoculated mice with that type of bacteria, the mice experienced less gut irritation and engaged in more social interaction.
The new results could ultimately lead to treatments that use gut microbes to alleviate GI symptoms and influence behaviors. “I think that this is a really important step therapeutically,” said June Round, PhD, a microbiologist at U of U Health and the senior author on the study, “because now we can start to assemble a therapy with organisms that we know to be safe.”